Integrated Telephony
Caller ID links to charts; record calls with summaries for accurate intake.
A third of U.S. healthcare dollars disappear into billing fees and clerical work. PBS EMR gives that time back with integrated telephony, voice‑first notes, one‑click claims, and direct‑to‑payer connections—so PTs, OTs, and SLPs spend less time on screens and more with patients.
Exact‑match pages help you compare workflows for each specialty:
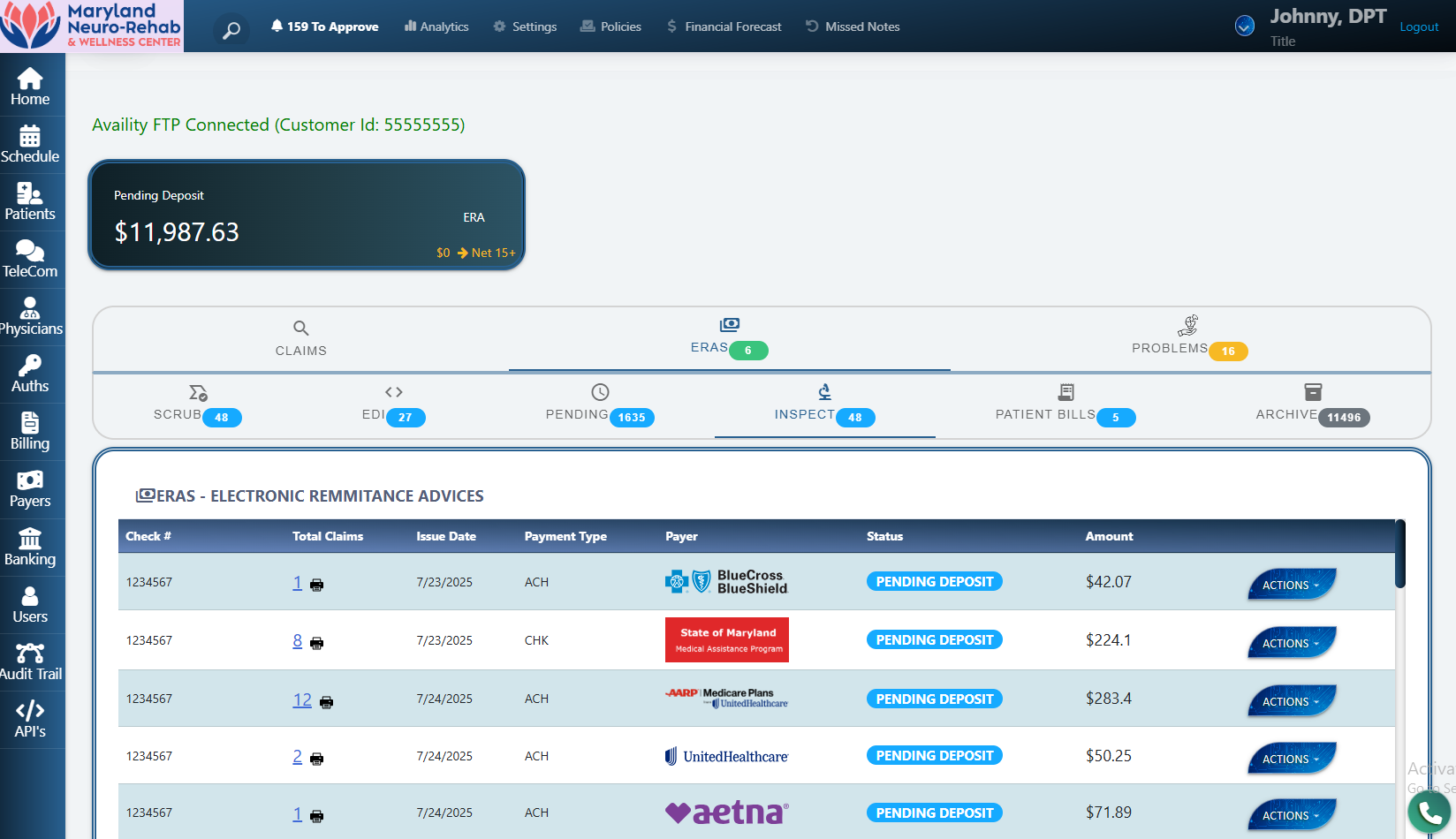
Traditional EMRs route claims through third‑party clearinghouses that add latency and fees. PBS EMR submits eligible claims directly to insurers, cutting payout cycles and erasing per‑transaction fees—while ERA auto‑posting and eligibility checks keep A/R clean.
Caller ID links to charts; record calls with summaries for accurate intake.
Auto‑verify addresses and 9‑digit ZIP for clean claim submissions.
Real‑time E&B in the chart; track visit limits, copays, deductibles.
One‑click NPI import; WC case module with templated fax packets.
Facility hours, providers, and rooms—next available in a click.
Track approvals/partials, dates, and remaining visits by policy.
Record the eval; AI drafts SOAP, plan of care, summaries, and HEP.
Tech/assistant inputs update next‑session steps automatically.
Flags CPT errors, duplicates, and auth gaps before submission.
Routes claims via the fastest channel; ERA posts and status sync.
Co‑pays at check‑in; statements & secure links; accurate balances.
Ask anything: days‑to‑pay, denials, capacity, and more—chat the data.
Yes. PBS EMR includes discipline-specific workflows and pages for Physical Therapy, Occupational Therapy, and Speech-Language Pathology.
Yes. PBS EMR can submit eligible claims directly to insurers and auto-post ERAs for faster reconciliation and fewer fees.
Yes. The chart-native AI is optional. It cites sources in the chart, flags gaps, and proposes next steps; you accept, edit, or ignore.
Teams switching to PBS EMR save 35+ admin hours per week and keep up to 12% more revenue—while spending more face‑time with patients.
Statements on time‑to‑payment and savings are based on internal implementations and may vary by payer and market.