Why is healthcare so expensive?
Short answer: too many toll booths, too many contradictions, and too much fragility. We’ve lived this as clinicians, billers, engineers—and we’re building differently.
Short answer: too many toll booths, too many contradictions, and too much fragility. We’ve lived this as clinicians, billers, engineers—and we’re building differently.
Patients pay high premiums and still fear surprise bills. Clinics fight through portals, phone trees, and conflicting answers just to get a clean claim out the door. Meanwhile, national health spending keeps climbing— it reached an estimated 17.6% of U.S. GDP in 2023 (CMS National Health Expenditure fact sheet).
We think the cost problem is simpler than it looks: too many middlemen, inconsistent rules, and fragile pipes add friction at every step—from eligibility checks to denials and appeals.
In HIPAA terms, a health care clearinghouse is an intermediary that converts or routes transactions between providers and payers (see the federal definition at 45 CFR 160.103). Every extra hop can add fees and time. When a major hub goes down, everyone pays the price: the Change Healthcare cyberattack caused widespread cash-flow disruptions, emergency policy responses, and congressional scrutiny (AP: lack of MFA on a key server; Reuters: hearings & data exposure; U.S. Senate Finance hearing page). CMS stood up accelerated and advance payments to keep providers afloat (CHOPD fact sheet; program closure update).
There are standardized code sets for denials (CARC/RARC), but they aren’t applied uniformly across payers in practice. That inconsistency creates busywork and back-and-forth phone calls to interpret what a denial really means. Industry efforts like CAQH CORE’s Uniform Use of CARCs & RARCs and its quarterly Code Combinations updates exist precisely to drive more uniform use across plans (CAQH CORE Operating Rules overview; Uniform Use rule (PDF); current Code Combinations list (XLSX); CMS contractor transmittal citing CORE 360 updates (PDF)).
Digital eligibility and benefits (the 270/271 “eligibility check”) helps, but the details still vary by payer and plan. Responses routinely include “not a guarantee of payment” language, so clinics often must call to confirm specifics like visit limits, exclusions, and carve-outs—especially for complex cases (CAQH CORE 270/271 data content rule (PDF); BCBSTX: “not a guarantee of payment”; HealthPartners EDI eligibility disclaimer).
Providers know the drill: complex forms, contradictory criteria, long waits, and “try again” answers. In the American Medical Association’s national survey, physicians overwhelmingly reported care delays and negative clinical impact from prior authorization (AMA 2024 press release; latest AMA survey PDF).
The Change Healthcare incident showed what happens when claims, eligibility, and remits depend on a few chokepoints. Policymakers pressed leaders on basic safeguards—like multi-factor authentication—during public testimony (AP report; Reuters hearing coverage; Senate hearing page). CMS and states even activated emergency measures to keep providers paid while systems recovered (CMS statement on accelerated/advance payments; Medicaid interim-payment flexibilities; CMCS informational bulletin (PDF)).
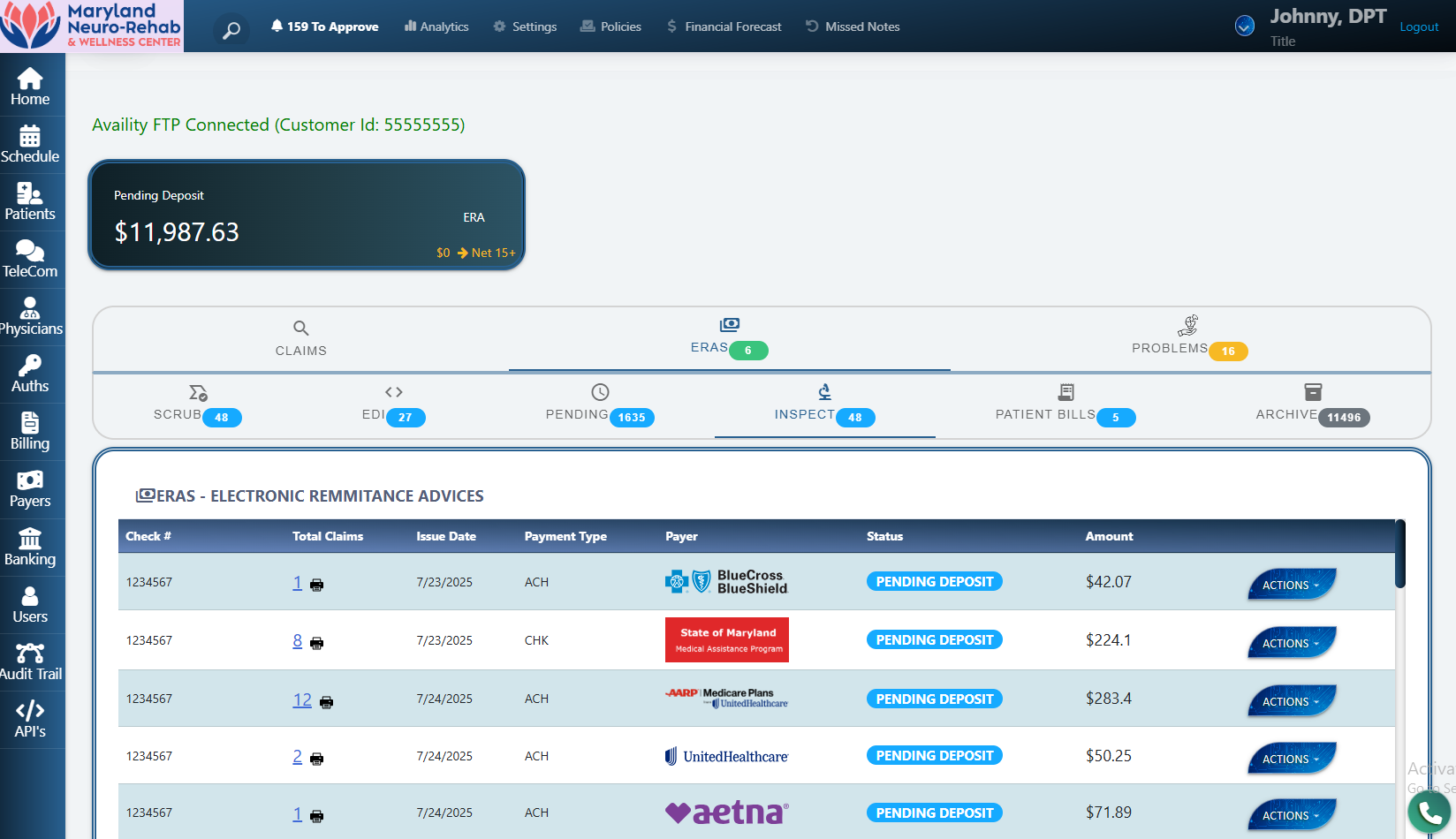
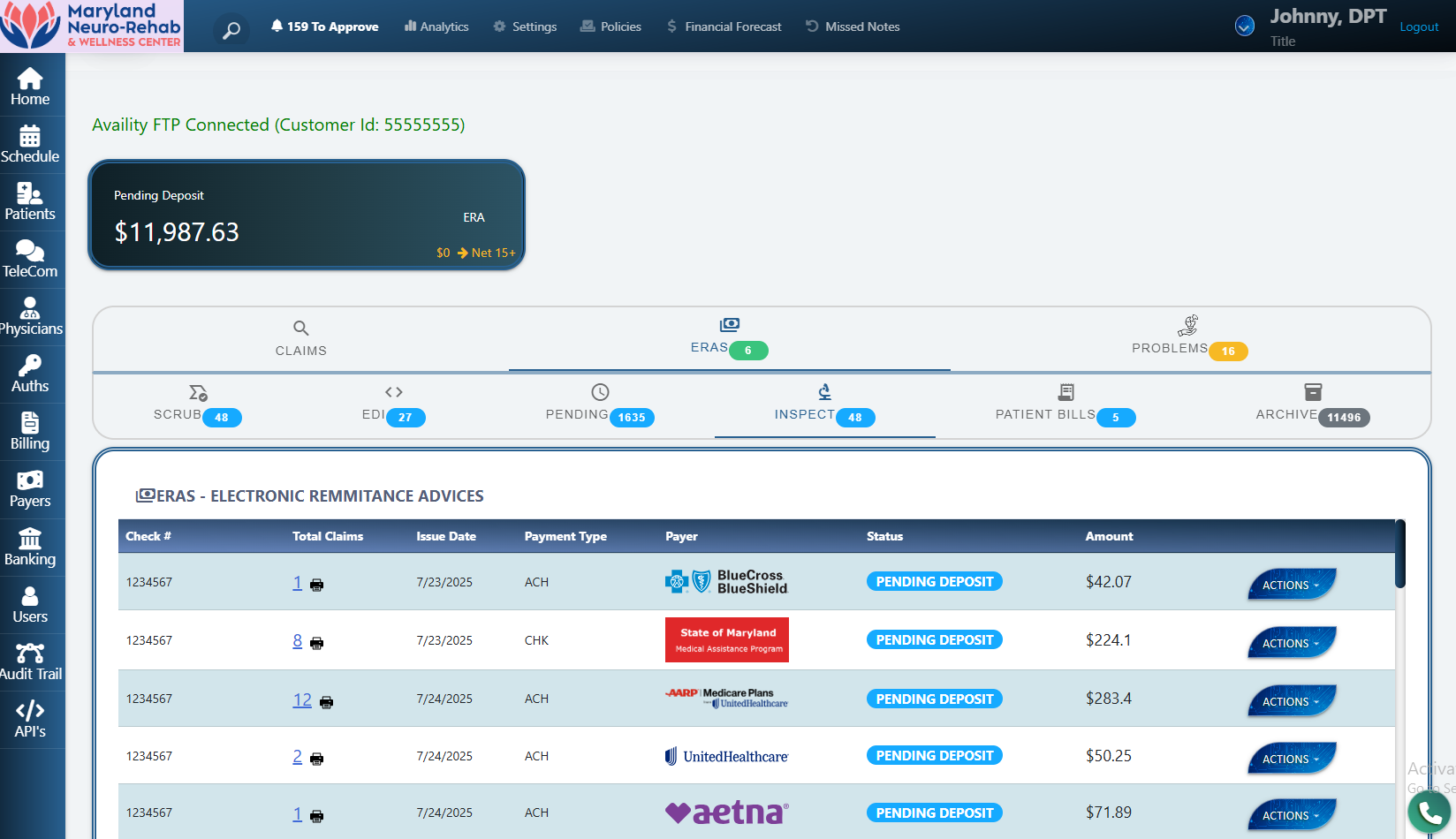
We’re unusual: our system operates as an EMR, a billing service, and a clearinghouse. That means fewer handoffs, fewer fees, and fewer chances for your claims to stall in someone else’s queue. Where payers support it and your enrollments allow, we submit direct-to-payer; where direct isn’t supported, we maintain clearinghouse routes as a backup.
Compliance note: HIPAA Administrative Simplification sets standards for electronic transactions (claims, remits, eligibility, etc.). See CMS overviews on transactions, operating rules and adopted standards. Connectivity and timing depend on payer policy and your enrollment. Education only—this is not billing, coding, or legal advice.
Want the deeper dive? See our feature deep-dives: Routing, Claim Scrubber, ERA Auto-Posting.
If you’re tired of middlemen, mixed messages, and waiting on hold, we’d love to show you a calmer way to run revenue.
Statements on savings and timing reflect our internal deployments and may vary by payer and market. This page is for education; it is not billing, coding, or legal advice.