Inbound & outbound in the chart
Caller ID resolves to patients; start an intake or open the chart instantly. Record calls with summaries so the story never gets lost.
An outcomes-focused therapy EMR built by clinicians and billing engineers. Explore the capabilities from call to cash—documentation, scheduling, billing safeguards, and direct-to-payer routing.
Caller ID resolves to patients; start an intake or open the chart instantly. Record calls with summaries so the story never gets lost.
Two-way texting for scheduling and logistics. Automated reminders reduce no-shows and smooth the day’s flow.
Capture demographics and payer info while you talk; push clean data into eligibility and scheduling.
Respect facility hours, provider availability, rooms, and equipment. Find next available in a click.
Visit counts, authorization windows, and plan rules surface before you overbook—no more surprises.
Collect copays at the front desk, issue receipts, and keep balances accurate from the start.
Store copays, deductible/OOP, visit limits, and policy notes directly in the chart.
Know remaining visits and dates at a glance. Stop over-treating before it becomes a denial.
Drafts SOAP, plans of care, and HEP from session context. You accept, edit, or ignore; sources are cited. Learn more.
Optional phrasing helps you stay defensible without slowing care—keep your clinical voice.
Inclusion cues and stop criteria can be embedded to support safe, reproducible handoffs.
Blocks mirror real PT/OT/SLP sessions—warm-up, targeted work, generalization, wrap-up—so documentation tracks what actually happened.
ROM/MMT, TUG, LEFS/NDI/ODI, intelligibility, FOIS, ADLs, and more map to interventions. Learn more.
Clear sets, inclusion cues, and stop criteria keep delegation safe and consistent across sites.
Duplicate/mutually exclusive CPTs, time-rule conflicts, missing/exhausted auths, and identifier issues are flagged in-chart. Learn more.
Send claims via the fastest reliable path—direct where eligible, clearinghouse fallback where required. Learn more.
Estimate billable units quickly. Open calculator (education only).
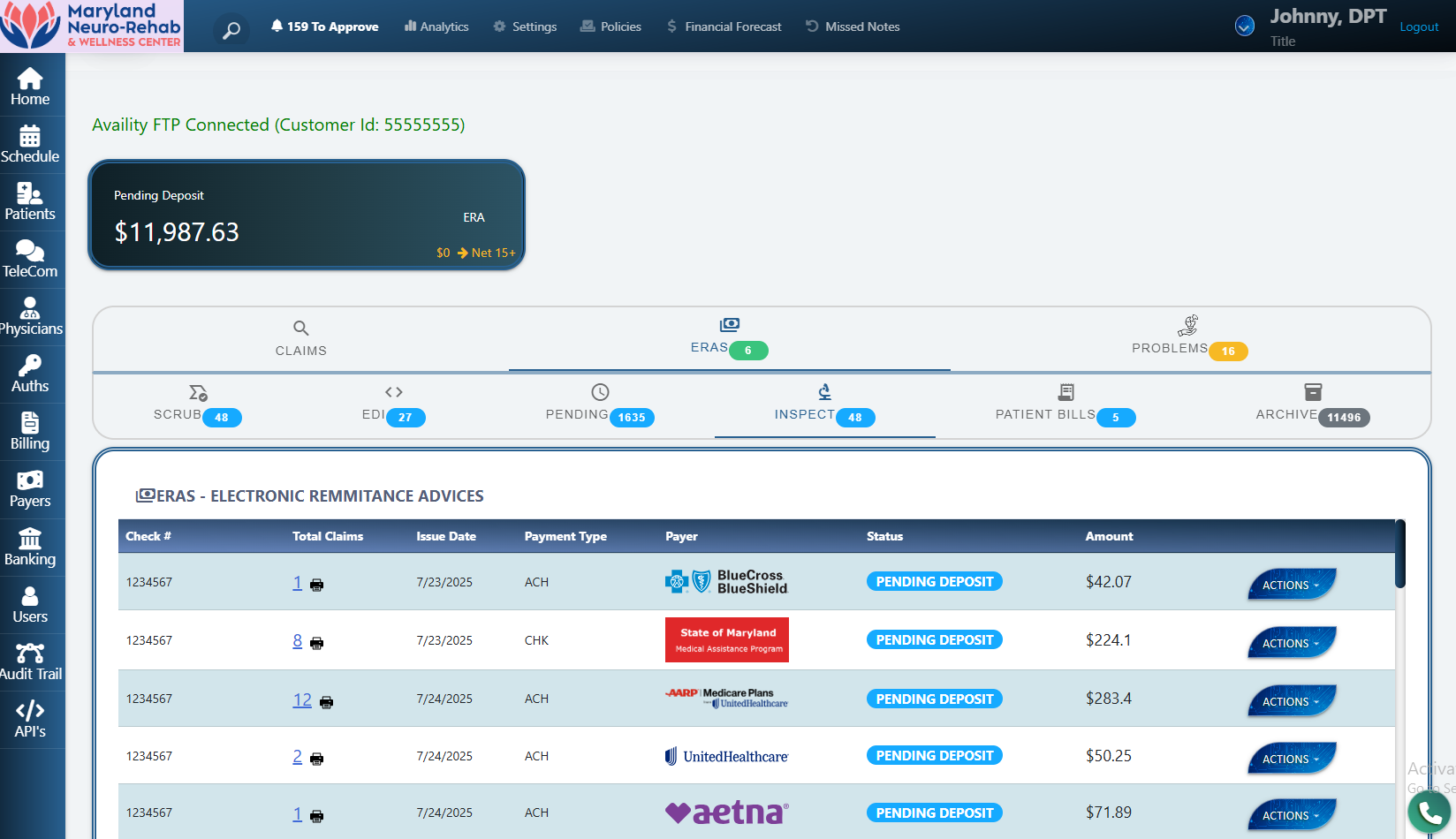
Map allowed amounts and adjustments to service lines; update patient responsibility. Learn more.
Clear statements with secure links; offer plans where appropriate. Accurate balances after ERA.
Queue COB follow-ups automatically after primary posting—keep the money moving.
Track adjusters, claim numbers, and requirements; generate templated fax packets in a click.
Keep approvals and documentation synced with visit counts and status.
ZIP+4 validation prevents address-related rejections at the source.
Pull provider/org NPI data into the chart and claims—no retyping.
Inbound faxes auto-file; outbound packets track delivery and confirmation.
Days-to-pay, denial classes, capacity, and trends—get dashboards and natural-language answers.
Tie outcomes to interventions and throughput so leaders can act with confidence.
Integrated telephony and intake feed directly into eligibility, visit management, documentation, billing safeguards, and direct-to-payer routing. ERA auto-posting and clear patient billing keep A/R clean.
Yes. PBS EMR includes discipline-specific workflows and outcomes-oriented documentation for physical therapy, occupational therapy, and speech-language pathology.
Yes. AI assistance is optional, cites the chart, and lets you accept, edit, or ignore suggestions.
Claims are routed via an optimized channel per payer—direct where eligible or through a clearinghouse otherwise—to reduce latency and fees.
Teams switching to PBS EMR save 35+ admin hours per week and keep up to 12% more revenue—while spending more face-time with patients.
Statements about time-to-payment and savings reflect internal implementations and may vary by payer and market.